Abstract
Large granular lymphocyte (LGL) leukemia is a spectrum of rare lymphoproliferative disorders. Two entities are reported: indolent T-cell LGL leukemia and aggressive NK cell leukemia. However, a review of the literature identified cases of aggressive T-cell LGL. Considering this unusual and rare clinical presentation, we are reporting a case of aggressive T-cell LGL leukemia.
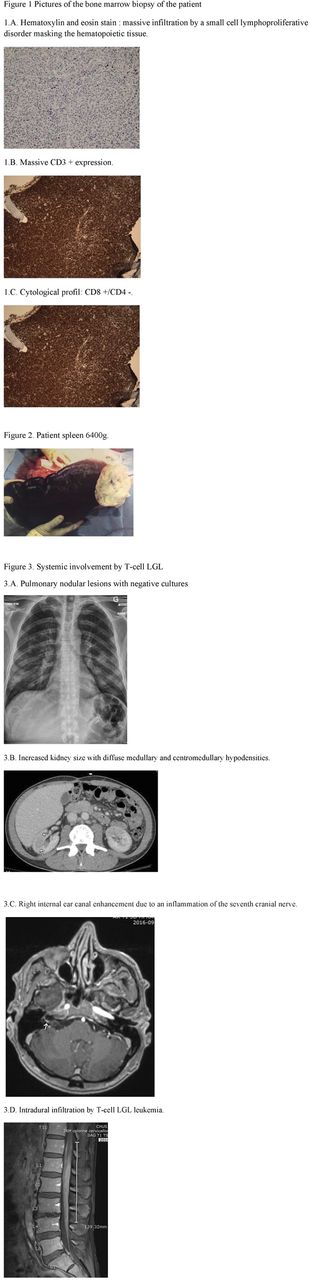
A 53-yo man presented in May 2014 with a one year history of constitutional symptoms, splenomegaly, mild lymphocytosis and a pancytopenia (hemoglobin 105 g/L, neutrophils 0,5 x 109 /L and platelets 80 x 109 /L). He had similar symptoms at the age of 24 that resolved without further investigation. Bone marrow evaluation revealed a massive infiltration by small to medium sized lymphocytes with irregular nucleus CD3 +, CD4 -, CD7 -, CD8 +, CD25 -, CD33 -, CD34 -, CD56 -, CD57 -, TCRαβ+. HTLV-1 serology was negative. His pancytopenia did not improve with 3 cycles of CHOP followed by 4 cycles of ESHAP. In January 2015, indolent T LGL was finally retained. The patient was observed up to July 2015 where methotrexate was begun because of frequent infections and symptomatic splenomegaly. A splenectomy was performed in January 2016 due to a toxicity to methotrexate and persistent symptoms from splenomegaly. Pathology report showed a splenic and lymph node infiltration by mature T CD8+ lymphocytes supporting the T LGL diagnosis. Post splenectomy, cytopenia improved and progressed in June 2016 with a lymphocytosis (82 x 109/L), new lung infiltrates and acute renal insufficiency. The lung biopsy revealed an infiltration by the T-cell LGL and renal imaging suggested infiltration by this T-cell LGL as well. Based on the weak expression of CD20+ on the splenic pathology, rituximab was attempted in August 2016. The patient rapidly progressed fatally with systemic involvement of T-cell LGL (skin, lungs, liver, kidney, facial cranial nerves, conus medullaris and bone marrow).
This case therefore depicts a very aggressive case of T-cell LGL with an atypical clinical presentation. In contrast to the indolent variant and as seen in the few similar cases retrieved in literature, the clinical presentation of the aggressive T-cell LGL leukemia is characterized by constitutional symptoms, rapidly progressive hepatosplenomegaly, cytopenia with/without organic infiltration and an important resistance to treatment. Moreover, concerning the pathological findings, the medullary involvement of our patient was massive without real images of intra-sinusal lymphocytosis and the T-cell of this T-cell LGL were atypical because of their small-medium size with slightly irregular nuclei and the lack of expression of CD56 and CD57. However, the few studies on aggressive T-cell LGL leukemia retrieved similar findings. Even though there is no consensus on the optimal therapeutic management of this disease, we believe that the treatments given to our patient were consistent with literature and did not add an additional mortality risk.
To conclude, LGL cell leukemia represent a spectrum of indolent and aggressive diseases, whereby an indolent form can evolve into an aggressive form. Aggressive T-cell LGL leukemia are characterized by a multisystem disease, an atypical immunophenotype (CD56-, CD57-) and are associated with an uncertainty regarding therapeutics.
Fleury: Gilead: Consultancy, Honoraria; Lundbeck: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Merck: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal